HPV infections drive increases in head and neck cancer
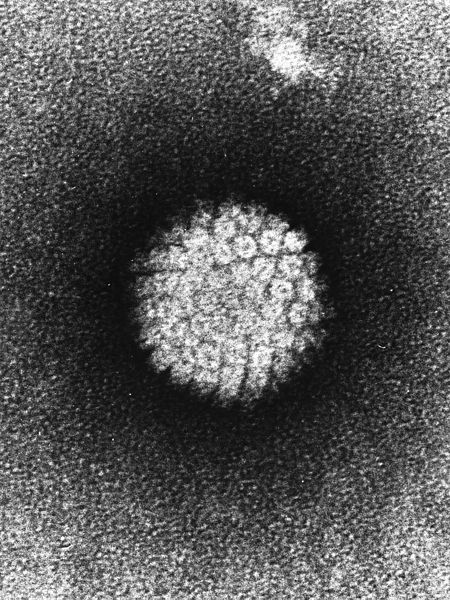
Electron micrograph of a negatively stained human papillomavirus. (Public domain image from Laboratory of Tumor Virus Biology, National Institutes of Health)
Human papillomavirus (HPV) is changing the face of head and neck cancer.
Once caused primarily by heavy tobacco or alcohol use, the majority of new head and neck cancers in the United Stated result from infection with HPV, a common sexually transmitted disease known for causing cervical cancer in women. As a result, head and neck cancer is increasingly being found in younger patients—especially men. And rates of diagnosis are on the rise.
“HPV might be driving dramatic changes in the incidence rates of head and neck cancer in the US population over a very short period of time,” said Maura Gillison, a medical oncologist at the Ohio State University Comprehensive Cancer Center, speaking at CASW’s New Horizons in Science briefing during the ScienceWriters2014 conference in Columbus, Ohio, on Oct. 19. “It’s a really remarkable and radical change.”
Head and neck cancer: a changed picture
Gillison has been studying the connection between oral HPV infections and head and neck cancers since doctors first observed an increase in the incidence of this disease in the 1990s. By testing tumor tissue from three population-based cancer registries in the United States, she and her colleagues found that the number of HPV-positive cases of head and neck cancer increased from 16 percent in the late 1980s to 72 percent by the early 2000s.
“The cancer that we were diagnosing and treating in the mid-1980s was a very different cancer… than the cancer we were seeing today,” Gillison told the science writers.
For example, HPV-positive cancers arise in the back of the throat and the tonsils, rather than in the mouth; they occur in younger individuals and are three times more prevalent in men then in women. The primary risk factors have also shifted, from tobacco and alcohol use to sexual behavior.
And the number of cases in men is rising so quickly that “by about sometime between now and 2020, there will be more men diagnosed with HPV positive cancer than women,” said Gillison.
Why are so many men affected?
According to Gillison, most sexually active people—both men and women—contract HPV at some point in their lives. Why, she wondered, are the rates of HPV-positive head and neck cancer increasing, and why are they higher in men?
To answer these questions, Gillison examined the prevalence of oral HPV infection within the United States as part of the National Health and Nutrition Examination Survey.
She found that around seven percent of the population had an oral HPV infection, and men were three to five times more likely to have one than women. The key difference was in the relationship between the number of sexual partners and oral HPV infection. In men, the prevalence of oral HPV increases with each additional sexual partner until it reaches a plateau at 30 partners. In women, this plateau arrives more quickly, after only three sexual partners. Gillison attributes the overall rise in HPV-related cancers to the sexual revolution, which made it socially acceptable for people to have more partners.
“Women got more partners, but after three they were protected,” said Gillison. “Men continued to be at risk.” This disparity likely arises because women are able to build up immunity to HPV, she said, while men are not.
Gillison said that understanding how HPV has changed head and neck cancer could also inform our approach to other types of cancer, such as the relation between hepatitis B and liver cancer. “There might be similar underlying shifts in other cancers that we just can’t appreciate, and it could have a profound impact on how we diagnose and treat cancers,” she said.